The National Patient Blood Management Collaborative (NPBMC) conducted by the Australian Commission on Safety and Quality in Health Care (ACSQHC) concluded in March 2017.
For the past two years Lismore Base Hospital, St Vincent’s Private Hospital and the North Coast Primary Health Network have been involved in the NPBMC, working towards identifying and managing pre-operative anaemia and/or iron deficiency in patients preparing for major elective bowel, gynaecological and joint replacement surgery. With a particular aim of avoiding blood transfusion, local NPBMC teams concentrated on engaging GPs in the Primary Health Network to optimise patients’ iron and haemoglobin status prior to surgery.
Although the Collaborative has come to a close, local data collection and further work in other surgical streams is ongoing. We aim to optimise pre-operative care for patients undergoing all types of major surgery by complying with the ACSQHC National Health Care Accreditation Standards.
As shown below, over the course of the Collaborative pre-operative iron deficiency assessment has markedly increased in both the primary and secondary sectors.
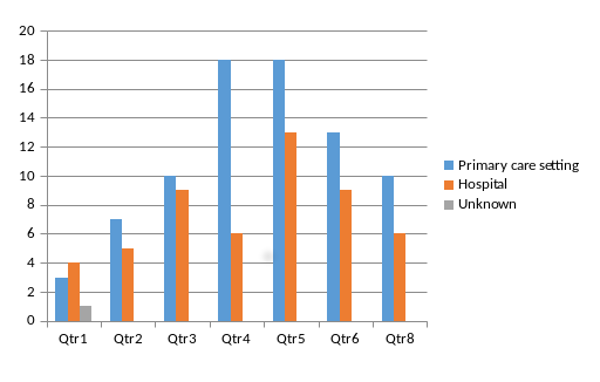
Site of pre-operative assessment for iron deficiency
Primary care led the way in pre-operative iron deficiency management, with the numbers rising steadily in the first half of the Collaborative.
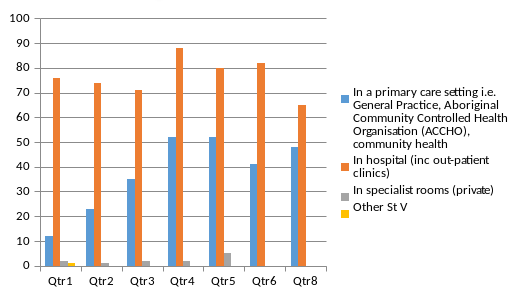
Site where iron deficiency was managed
When analysed by surgical cohort, iron deficiency management in the gynaecological and orthopaedic streams was well managed in primary care.
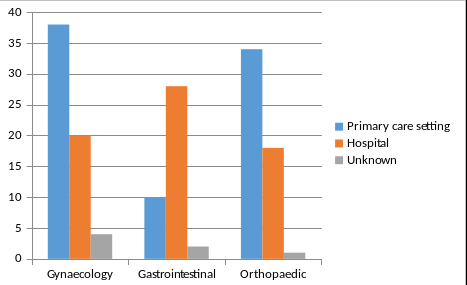 Site where iron deficiency was managed (by surgical stream)
Site where iron deficiency was managed (by surgical stream)
Conversely, hospital services managed 70% of identified iron deficiency in patients undergoing gastrointestinal surgery. This may be due to the often short time to surgery after a colonoscopic diagnosis that requires surgical intervention.
In an effort to address these findings, a management point has been added in the Mid and North Coast NSW, Health Pathways: Bowel Cancer Symptoms (Management Point 2).
If iron deficiency identified, consider commencing iron replacement, as this will not affect results of colonoscopy, and will lead to improved outcomes if surgery is required. If rapid iron replacement is required, see Iron Infusion.
Hospital services have limited capacity to provide iron infusions. Undertaking iron infusions in general practice contributes to improved care and less waste in the hospital system.
The Northern NSW Local Health District is able to assist general practices with implementing iron infusions in their surgeries. Local Clinical Nurse Consultant for Blood and Blood Products, Beverley Hiles, is now available for onsite general practice visits.
Visits can be organised to minimise disruption to practitioners' schedules and are tailored to the particular needs identified by the practice. Topics for practices to consider include:
- evidence based practice protocols for iron administration
- iron management guidelines for staff
- patient information pamphlets and consent sheets
- iron studies interpretation guides
- cannulation training
An excellent resource for general practitioners is Dr Pradeep Jayasuriya’s informative discussion on iron deficiency, at the recent Adelaide Iron Symposium: From Primary to Tertiary Care, June 3rd 2017, where he shared his experience of setting up iron infusions in general practice.
General practices interested in undertaking or improving their iron administration capacity can contact Beverly Hiles at





