Preoperative iron management has improved on the North Coast in the last 18 months. However there is still room for further improvement, particularly in major bowel surgery. The local co-ordinator of the project, Beverley Hiles, reports on progress to date.
The Australian Commission on Safety and Quality in Health Care has been conducting the National Patient Blood Management Collaborative (NPBMC) since July 2015. Lismore Base Hospital and Lismore St Vincent’s Private Hospital along with the North Coast Primary Health Network have been a part of this national collaborative.
The aim of the collaborative is to identify and manage preoperative anaemia and/or iron deficiency in patients scheduled for elective surgery where significant blood loss could occur, namely in gynaecological, gastrointestinal and orthopaedic surgical streams. It is a key patient blood management strategy for optimising red blood cell mass before surgery while aiming to reduce blood transfusion which may be an independent risk factor for increased morbidity and hospital length of stay.
Our focus on the North Coast was to engage GPs in optimizing a patient’s blood prior to surgery as we recognized that GPs are best placed to manage iron deficiency and anaemia and would play an important role in the collaborative.
Letters are sent to GPs once the hospital has a request for admission for the selected surgical groups, requesting preoperative assessment and management of anaemia and/or iron deficiency ahead of surgery.
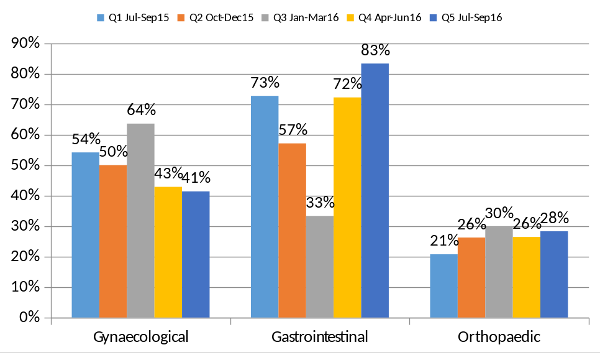
The results to date show a promising upwards trend for iron deficiency assessment and management throughout each quarter of data collection.
Graph 1 illustrates a steady increasing trend in iron deficiency management in the primary care setting.
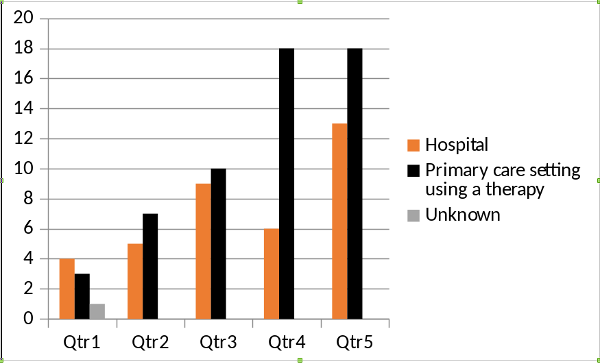
Graph 1: Where was iron deficiency managed
Graph 2 demonstrates that although there is an increasing trend in primary care in the assessment of iron deficiency preceding surgery, 60% of iron assessment by the 5th Quarter is still performed by hospital services at the preoperative assessment clinic.
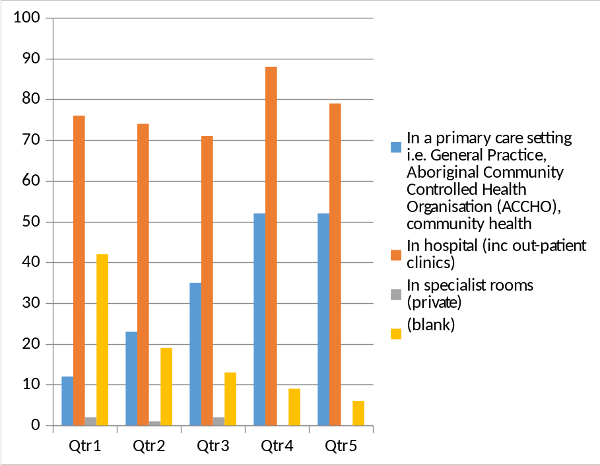
Graph 2: Iron deficiency assessment
Following an in-depth discussion between the NPBM and national teams on management of iron deficiency and anaemia, teams undertook a small audit of non-managed iron deficiency to better understand why management was not recorded and to identify potential areas for improvement.
Some management factors identified were:
- a decision not to treat borderline results
- unawareness of the impact of iron deficiency in the absence of anaemia
- or lack of acknowledgement that there may be iron deficiency if haemoglobin is within range.
Table 1 from the Australian Red Cross Blood Service explains the spectrum of iron deficiency, highlighting that normal range haemoglobin can be maintained in iron depletion and iron deficient erythropoiesis. It is possible therefore for a patient facing major surgery where bleeding may occur, to be iron deplete with normal haemoglobin, and reliance on FBC alone may be a less favourable option in the preoperative care process. See the Spectrum of Iron Deficiency
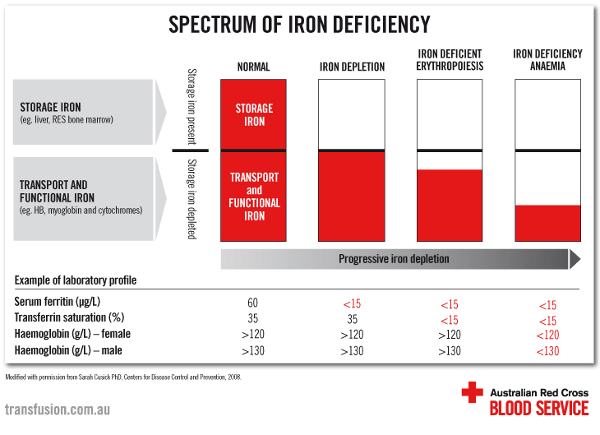
Table 1: Spectrum of Iron Deficiency
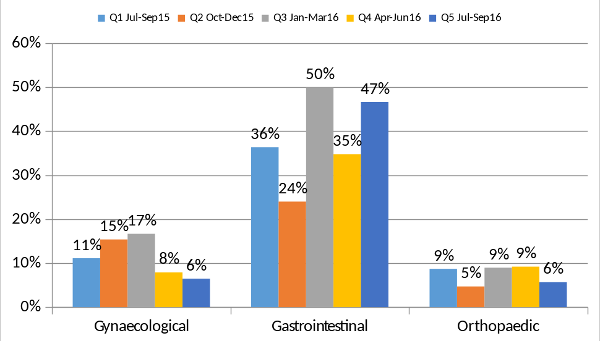
Our local data in Graphs 3 and 4 indicates also that while anaemia may be present in each surgical cohort, iron deficiency is more prevalent and may be present without anaemia.
Graph 3: Confirmed Anaemia
Graph 4: Confirmed Iron Deficiency
Current guidelines from the National Bowel Screening Program recommend checking iron studies for iron deficiency prior to colonoscopy/cancer screening. Our local NPBMC team advocates early iron replacement in iron deplete patients referred for gastrointestinal surveillance, as iron management will not alter the outcome of any investigations and will optimize the patient should surgery be required.
GPs interested in further information on correcting iron deficiency are referred to the excellent, well written and easy 6 minute read. ‘Correcting iron deficiency’ in the Australian Prescriber, Volume 39: Number 6: December 2016. Correcting Iron Deficiency




