“Plan for the worst. Hope for the best. Use the experience and resources for the future”
Versatility/Capacity
The COVID-19 action plan activated across the Northern NSW Local Health District included:
• Increasing capacity to treble the number of ventilated beds
• Using a separate ICU with negative pressure rooms
• Creating admission and assessment pathways for patients according to severity of their illness while reducing the risk of exposure to the public, staff and emergency department.
• Managing patients in the community according to severity stratification and risk factors for deterioration in Hospital in the Home (HITH) in concert with GPs.
• Managing patients using novel assessment processes (home oximeters and pulsimeters), and using markers of severity (Lactate, O2 sat, D-Dimer, Troponin, Urea, LDH, Lymphocyte to Neutrophil ratios etc.)
Strengths & Weaknesses
Lismore Base Hospital (LBH) was fortunate to have the recent addition of a new ICU and ward block that contained many single and negative pressure rooms. Old wards earmarked for refurbishment or closure were quickly turned into a possible COVID-19 cohort ward.
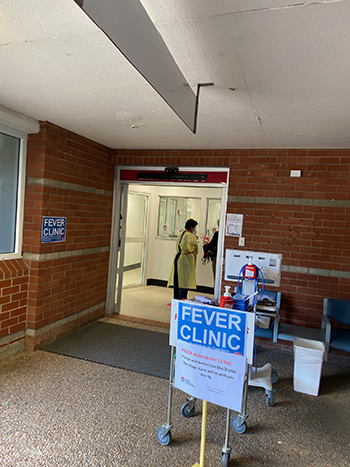
The old emergency department (ED) was used as the elective outpatients assessment clinic, and quickly turned into a “fever clinic” for testing for COVID-19. Its proximity to the HITH service allowed for easy assessment of patients requiring review.
A large waiting area and internal seating allowed for many to appropriately social distance. Televisions helped patients pass the time. A negative pressure room was earmarked in case a surge in the number of probable Covid-19 patients occurred.
All screened patients were logged into the electronic medical record, making. it is thus easy to admit those who returned positive swabs to HITH.
The use of a drive-in testing facility at LBH was considered but deemed impractical due to likely traffic issues near the new ED and car park.
Champions & Challenges
The Clinical Lead had public health and infectious diseases qualifications and previous experience in setting up screening clinics.
The traditional outpatient setting for the clinic , rather than a drive-through service, meant an increase in the amount of PPE used initially. As staffing levels increased and the clinic moved to a nurse-led model there was better use of resources and increased surge capacity.
Communicating a negative result proved difficult initially because of the volume of testing and confusion by the public on recommended screening practices. SMS communication was initially trialled using the Telstra Integrated Messaging service, however the slow turn-around times from reference laboratories resulted in some false negatives. A labour intensive system offered by the Sexual Health Service was subsequently replaced with Pathology North’s system, which proved to be reliable and error free.
As part of the clinic’s push to increase efficiency and develop a more streamlined approach to managing the clinical load we created written resources to reduce repeating the information given verbally.
We informed clinical staff elsewhere in the hospital that we were focussed solely on screening for COVID-19 and it was not appropriate for us to assess the cause of any fever. However, we emphasised our clinic was the right place to undertake screening noting that testing in the community is expensive and difficult due to the fact that using personal protective equipment is cumbersome and the required cleaning is time consuming.
Reconfiguration of exit bollards to protect patient transport staff and public from patients entering for review from HITH or exiting from screening was required. Donning and doffing and assessing unwell patients in their homes proved challenging. A national HITH email group and webinar HITH COVID-19 meetings were convened to share experiences, resources and service structures. It was comforting to learn our service structure was similar to others and we all had similar challenges.
Stakeholders & Resources
Close contact with Public Health and Pathology North ensured that all individuals with COVID-19 were assessed for risk of deterioration and were admitted to their nearest HITH program (Tweed or Lismore). The program ensured that appropriate contact tracing and testing of contacts occurred. Multiple federally-funded testing clinics were established around the area and some GP practices also set up COVID-19 testing clinics to service their patients. Some of these were of the “drive through” style.
Next Phase
The Australian and North Coast response to COVID-19 has been highly successful but the future course of the pandemic is unknown. We are prepared for four possible scenarios.
1. No “second wave” of COVID-19. In this scenario testing is ramped up to include sentinel asymptomatic sections of the community to monitor transmission. Antibody testing is used to assess asymptomatic transmission. This testing may transition to GP respiratory clinics which can also assess for influenza and other viral infections as part of their management of respiratory illnesses in winter.
2. Small outbreaks of local transmission. The current system identifies mildly symptomatic contacts. This too could transition to GP-based testing clinics.
3. “Second wave” hits. In this scenario the full Local Health District plan is implemented. COVID-19 HITH is utilised. GPs will look after milder cases and transition to HITH or hospital should they deteriorate. COVID-19 single rooms to be used in LBH and the separate COVID-19 ICU activated.
4. Major infection wave occurs nationally. Separate planned COVID-19 ward opens. Current plan is revised to cope with increased pressure on the existing model.
Covid-19 Response from Around the World
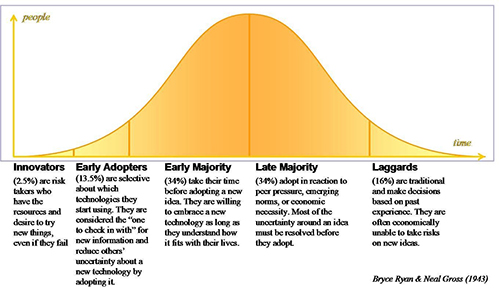
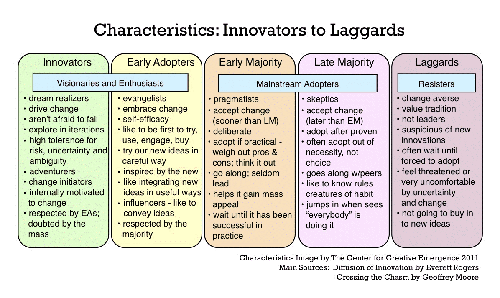
An interesting concept to apply to public health and other interventions is Everett Rogers’ Diffusion of Innovation paradigm.
It is possible to think of a country’s response to an epidemic using this paradigm for their compliance with social distancing and stay at home orders and their establishment of Hospital in the Home COVID-19 programs, COVID-19 screening programs and the setting up inpatient COVID-19 services.
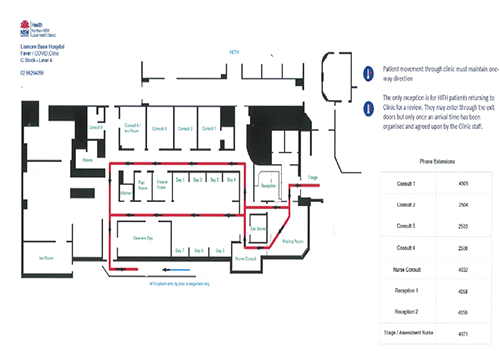
Here is the outline of outpatient floor plan and flow for our new service at LBH.
Flow of Patients attending for COVID1-19 testing or review in HITH (see below)
1. Triage – RN or EEN triage patients on arrival.
2. Reception – Ward Clerk “naps” the “non admitted patient” in.
3. Waiting Room – after patients have been NAPed in they are asked to enter the waiting room.
4. Doctor / Nurse Consult – RN or EEN review patient and swab.
5. Bays 1 to 7 – If the waiting room fills up. Staff escort patients from the waiting room to ancillary bays for ongoing patients to enter through reception.
6. Day Stores – PPE is stored.
7. Consult Rooms 1 to 5 - Doctor / Nurse Consult – DR, RN or EEN review patient and swab.
8. Cleaner’s Bay – Cleaner attends to areas after the patient leaves the waiting / bay seating area and the consult room before the next patient is assessed.
9. Patients exit through the side door along the barriers to the stairs.
10. HITH patients are not seen in the main clinic but enter via “the exit” after notifying staff by phone prior to entering.