There have always been demands for efficiency in health care and this only seems to increase. Year after year, the Australian health budget grows by a greater percentage than GDP and this is not sustainable. The COVID-19 pandemic has further increased the need for efficient delivery of medical services. Local disasters like the steriliser breakdown in Grafton or the terrible floods in Lismore and surrounds further blow our surgical waiting lists out.
I have been in Northern NSW for a bit over 10 years but it wouldn’t be a surprise if waiting lists for elective surgery in the public system are as bad now as they have ever been. That also has flow on effects for the provision of care in the private system, where especially in Victoria, significant private capacity has been used for the provision of public elective surgery.
There is clear impetus for change here. As clinicians though, improvements to our models of care ideally arise in a patient focused manner with the motivation being to do the best we can for the patient in front of us. In many cases that will also result in more efficient health care. Day-only total joint replacement is an exciting example where patient centered concerns align with a benefit at the health resource level.
This is not ground-breaking stuff. It is self-evident that, all other things being equal, it is both a better patient experience and more cost effective if a patient recovers from (say) pneumonia more rapidly rather than more slowly. So why, aside from a few isolated pockets of ERAS (enhanced recovery after surgery) programs, aren't we seeing more of a concerted effort to have people recover more rapidly after surgery?
This may be down to a misunderstanding. Many clinicians are under the mistaken impression that ERAS and day surgery total joint replacement programs are tricks to cut costs or otherwise under-service patients and then somehow still salvage an acceptable outcome.
Clinicians suspect that day surgery programs or short stay programs are health resource focused rather than patient centered. Others may believe that we are discharging patients who really require inpatient care, but somehow recreate the hospital environment at home with super resources. Neither of these is the case.
A unit that is trying to discharge patients who aren’t discharge-ready and then make up for it is probably going about day surgery the wrong way.
I recently had the pleasure of presenting a NORDOCs webinar on the day surgery total knee replacement (TKR) pilot program that commenced in August 2020 at Grafton Base Hospital. We combined the results with a number of self-funded, day surgery TKR patients from the private system and compared these to the overnight patients from the same time period.
It is worth pointing out that other than the day of surgery discharge and one extra visit to the office for pain catheter removal, the day surgery and overnight patients had equivalent and standard care with standard resources.
There are multiple small interdependent and cumulative factors that all contribute to a successful day surgery model of care. That in itself is a very interesting area. There is certainly no one key thing. In TKR surgery, a less invasive approach, minimal tourniquet use, thoughtful local anaesthetic infiltration, intra-articular anaesthetic catheter, generous use of corticosteroid, novel bandage technique and an appropriate anaesthetic are all examples of steps that contribute in our unit, along with many other details which are minor in isolation.
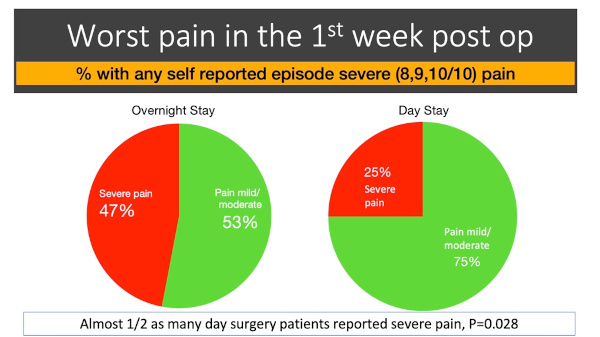
There were 17 day surgery patients and 100 overnight TKR patients. Since then, the day survey cohort has grown by 7 to 24. The day surgery patients were found to be more likely to be satisfied with the process, and more likely to recommend the process to a friend or family member. The day surgery patients also reached greater levels of function at an earlier time point than the overnight patients. Missing out on inpatient rehabilitation did not appear to compromise their recovery. Of particular note, the day surgery patients were half as likely to report an episode of severe pain in the first week after surgery. It turns out that analgesia still works at home!
With further research, this may become clearer. At the moment, it appears that if anything, post-surgical analgesia is more efficacious at home with patients who are less sleep deprived, more comfortable, have more to occupy them and aren’t constantly questioned about their pain.
Hospitals as we know them are safe places to be for sick people, but aren’t necessarily the ideal healing environment to recover from a straightforward and reproducible surgical event.
The day surgery group also had a lower rate of presentations to emergency after the surgery than the overnight group and there were no readmissions in the day surgery group. Only one patient intended for day surgery failed to meet the discharge criteria on the day.
There is clearly some selection bias at play, but that speaks to the process as patients were selected prior to the surgery. Numbers in the study were too low for robust conclusions, but overseas studies with large numbers have shown the safety of day surgery total joint replacement.
Day surgery TKR clearly isn’t for everyone. The starting point though, of “what can we change so that patients recover more rapidly after surgery?” does apply to everyone.
In fact, it is likely that the patients who are not candidates for day surgery TKR - for example the very elderly, frail and those with significant comorbidity - are the patients who have the most to gain from surgery undertaken in a manner which is associated with a more rapid recovery and is easier to get over in general.
After all, the physiological insults associated with TKR are simple. These are blood loss (which can be minimised), pain (which can be minimised), a period of immobility (which can be minimised) and anaesthetic/analgesic side effects (which can be minimised, especially if pain is minimised).
It is time for arthroplasty surgeons in Australia to catch up with the rest of the world, where in many cases day surgery total joint replacement is a standard model of care.
It is not only patients in the USA or Europe who would like to recover from surgery with less pain and regain independence and function more rapidly. Ours do too. Ultimately the exact date of discharge isn’t important, but more efficient use of our overloaded hospitals is a welcome byproduct of protocols that facilitate an enhanced recovery after surgery and that is good for everyone.
I would like to acknowledge my colleague orthopaedic surgeon Dr Michel Genon, Dr Alan Tyson, director of anaesthetics at Grafton Base Hospital, Amanda Tutty, director of physiotherapy, and Dr Corey Scholes of EBM Analytics for their contributions.
















