Doctors informed about new abortion law
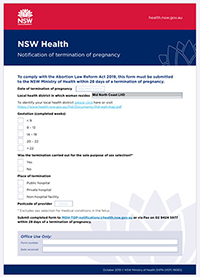
In a “Dear Doctor” letter to the state’s medical practitioners the NSW Health Secretary Elizabeth Koff has advised that the Abortion Law Reform Act 2019, passed on 2 October after criticism by objecting MPs and their supporters, means that terminations are now legal but must be reported within 28 days of the procedure.
The single-page notification form requires information on the LHD in which the woman resides, the gestation of the foetus - ranging from under 9 weeks to 22 weeks, after which special conditions apply - where the termination took place (public or private hospital, or non-hospital facility), the postcode of the provider, and perhaps more controversially, whether the termination was carried out “for the sole purpose of sex selection”, unless the foetus had medical conditions.
During the acrimonious debates that preceded the bill’s passing a number of critics suggested that certain ethnic communities preferred male children and would seek to abort girls.
- Details

Drink makers resist warning of pregnancy risks
While the government considers mandatory bottle warning labels about the risks of alcohol to unborn babies, the alcohol lobby is reacting in a similar way to tobacco marketers more than twenty years ago.
Food Standards Australia and New Zealand (FSANZ) has released a draft label for alcohol bottles, with a graphic showing a silhouette of a pregnant woman and the message, ‘‘Health warning: Any amount of alcohol can harm your baby’’.
Submissions to the FSANZ process closed on 4 October 2019.
Both governments advise women not to consume any alcohol during pregnancy: “Exposure of the foetus to alcohol can cause a range of physical, cognitive, behavioural and neurodevelopmental disabilities, collectively known as Foetal Alcohol Spectrum Disorder (FASD).”
Simply put, “FASD is preventable by avoiding alcohol consumption during pregnancy.”
- Details

ACON wants to help GPs with sexual and gender health
Not many years ago a diagnosis of HIV-AIDS was generally regarded as a death sentence, and many gay men, or men who had occasional sex with men, began planning for the end of their days. Hoping to make the most of the time left, a good number sold up down south and moved to the NSW Northern Rivers, a place of tolerance, cultural and climatic appeal, and decent health services.
Most expected to die, but one of those rare medical ‘miracles’ occurred, slowly at first, as is the way with research, and then picked up pace: treatments for the HIV virus, and more recently, preventative medications, were developed, found successful, and became widely available. Today, the anti-viral prophylactic PREP and the ‘morning after’ pill PEP, both prescribed by GPs, are the new normal.
- Details
Read more: ACON wants to help GPs with sexual and gender health
‘Break it down’ Aboriginal youth program funded
North Coast Primary Health Network is partnering with local organisation Desert Pea Media (DPM) to produce a social and emotional wellbeing program worth $800,000 to support local Aboriginal communities.
Young Aboriginal people on the North Coast experience disproportionate levels of mental health issues, including self-harm and suicide while cultural continuity and self-determination are protective factors for Aboriginal and Torres Strait Islander peoples' social and emotional wellbeing.
Since 2002, DPM has worked with Indigenous young people across Australia using contemporary storytelling techniques and audio-visual media to facilitate important social and cultural conversations. Working collaboratively with Elders, young people, community leaders and local service providers, DPM’s Break It Down is an Aboriginal youth mental health literacy program. The program is relevant and appropriate to the needs of individuals and communities.
Break it Down provides a safe space for young people to express themselves about difficult topics like mental health, and the use of alcohol and other drugs.
- Details

Health from the Grassroots
Aboriginal health priorities project Northern Rivers, NSW
Aboriginal staff at the University Centre for Rural Health (UCRH) in Lismore are leading the Health from the Grassroots Project aimed at giving voice to local mobs (from the Tweed to Clarence Valley) to talk about their priorities for community health and wellbeing and perspectives on what’s working well and what needs improvement to support community health and happiness.
We aim to collate the many comments and feedback received into actions to inform service provision and research.
- Details
Page 68 of 177















