A new report billed as a ‘landmark’ in Australian research has warned that the current over-use of antibiotics could send the nation, and by extension the wider world, back to the days before modern medicine - the Dark Ages.
The Antimicrobial Use and Resistance in Australia (AURA) 2016 report was produced by the Australian Commission on Safety and Quality in Health Care. This Australian Government agency leads and coordinates national improvements in the safety and quality of health care based on the best available evidence.
Its Senior Medical Advisor Professor John Turnidge said the study will inform action to prevent the spread of antimicrobial resistance [which] is “one of the most significant challenges for the delivery of safe, high-quality health services, and has a direct impact on patient care and patient outcomes.”
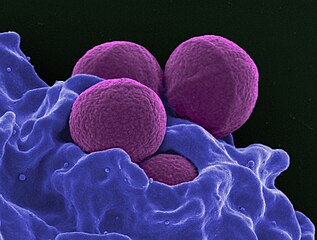
He added, “Antibiotic resistance has developed because of the overuse and misuse of antibiotics, and now, bacterial infections that were once easily cured with antibiotics are becoming harder to treat.”
According to the AURA 2016 report, nearly half of all Australians were prescribed antimicrobials in 2014, however a significant proportion did not need them. In hospitals on any given day, more than one-third of patients were given antibiotics, with almost half either inappropriately prescribed or flouting guidelines.
Prof Turnidge warned that, “We should all be very concerned. We are already seeing superbugs in the community ... and outbreaks in hospital wards, where the amount of time and energy just to save those people’s lives is huge.”
Professor Chris Baggoley, Australian Government Chief Medical Officer, added, “Comprehensive, coordinated and effective surveillance of antimicrobial resistance and antimicrobial use is a national priority and a critical component of the Australian Government’s National Antimicrobial Resistance Strategy.
“The AURA project is extremely important in our fight to halt the progress of antimicrobial resistance, to ensure that we protect the safe and effective antibiotics that we rely on today.
“This report represents a milestone; it explores patterns in prescribing and use of antibiotics, to understand where and when specific threats emerge – the kind of information we need to guide efforts to mitigate the risk of antimicrobial resistance at a local, jurisdictional and national level.”
Key findings from AURA 2016:
- In 2014 10.7 million Australians were prescribed antimicrobials – 46% of the population.
- In 2014, Australia had one of the highest rates of vancomycin resistance Enterococcus faecium in the world. Resistance to ampicillin was even higher in this species.
- Antimicrobial resistances are having a major impact on seriously ill patients in hospitals and require major efforts in hospitals to control their spread.
- On any given day in an Australian hospital in 2014, 38.4% of patients were being administered an antimicrobial. Of these, 24.3% were noncompliant with guidelines, and 23% were considered inappropriate.
- Antibiotics used in surgery are often not required and are given for too long. In 2014, 40.2% of surgical prophylaxis was inappropriate, mainly because of incorrect duration (39.7%); incorrect dose or frequency (15.7%); or lack of documenting the reason (22.9%).
- Data on antimicrobial prescriptions show strong seasonal variance, with some antimicrobials being prescribed more in winter. Colds and flu are viral infections, and antibiotics do not help treat viruses.